Lost Human Capital From Early-Onset Chronic Depression
Abstract
OBJECTIVE: Chronic depression starts at an early age for many individuals and could affect their accumulation of “human capital” (i.e., education, higher amounts of which can broaden occupational choice and increase earnings potential). The authors examined the impact, by gender, of early- (before age 22) versus late-onset major depressive disorder on educational attainment. They also determined whether the efficacy and sustainability of antidepressant treatments and psychosocial outcomes vary by age at onset and quantified the impact of early- versus late-onset, as well as never-occurring, major depressive disorder on expected lifetime earnings.METHOD: The authors used logistic and multivariate regression methods to analyze data from a three-phase, multicenter, double-blind, randomized trial that compared sertraline and imipramine treatment of 531 patients with chronic depression aged 30 years and older. These data were integrated with U.S. Census Bureau data on 1995 earnings by age, educational attainment, and gender.RESULTS: Early-onset major depressive disorder adversely affected the educational attainment of women but not of men. No significant difference in treatment responsiveness by age at onset was observed after 12 weeks of acute treatment or, for subjects rated as having responded, after 76 weeks of maintenance treatment. A randomly selected 21-year-old woman with early-onset major depressive disorder in 1995 could expect future annual earnings that were 12%–18% lower than those of a randomly selected 21-year-old woman whose onset of major depressive disorder occurred after age 21 or not at all.CONCLUSIONS: Early-onset major depressive disorder causes substantial human capital loss, particularly for women. Detection and effective treatment of early-onset major depressive disorder may have substantial economic benefits.
Many young adults pursue further education after high school graduation. By foregoing current income and incurring the tuition costs of higher education, these individuals invest in their futures. This foregone income and higher education cost may be considered a form of human capital investment and accumulation. Payoffs from these human capital investments include increases in expected subsequent productivity and earnings (1).
The ability of young adults to successfully accumulate human capital depends in part on their health status during the years in which most post-high-school education typically occurs, i.e., ages 18–30. Illnesses with an early age at onset that substantially reduce physical, social, or cognitive functioning are particularly burdensome. The costs of such disorders include not only direct and indirect medical costs but also costs associated with reduced functioning and impaired ability to accumulate human capital. Detection and effective treatment of such early-onset disorders could reduce these costs.
This study examines the impact of early-onset major depressive disorder. About 15.7% of the U.S. population is estimated to have experienced an episode of major depressive disorder between the ages of 15 and 24, with a higher incidence seen in young women than in young men (20.8% versus 11.0%) (2). Depression produces similar or greater functional impairments than many other episodic and chronic medical illnesses (3–9). Depression is frequently underdiagnosed and inadequately treated (9–18). Guideline-consistent treatments for episodic depression produce success rates of 60%–70% for those patients who complete a trial (18–20). Moreover, antidepressants have been shown to be effective in the prophylaxis of recurrent mood disorders (21, 22).
This study reports the impact of early- (before age 22) versus late-onset—as well as never-occurring—major depression on human capital accumulation. Four issues are addressed: 1) Does early-onset major depressive disorder reduce educational attainment more than late-onset major depressive disorder? 2) Do human capital impairments associated with early-onset major depressive disorder vary by gender? 3) Do the efficacy and sustainability of antidepressant treatments for chronic depression and the psychosocial outcomes vary by initial age at onset? 4) Among individuals in the United States in 1995 who were 21 years of age, what are the differences in future lifetime expected mean earnings, by gender, attributable to lost human capital for those who experienced early-onset major depressive disorder versus those in whom it occurred later or not at all?
Method
The data for this study were derived from two sources: 1) a clinical trial that involved 635 chronically depressed outpatients; and 2) the Current Population Survey, which was conducted by the U.S. Bureau of the Census in March 1996.
Clinical Trial Data
A 12-site, double-blind, randomized, parallel-group trial compared the efficacy of sertraline and imipramine in the acute and maintenance treatment of 635 outpatients, aged 21–65 years, with DSM-III-R-defined chronic major or double depression (23, 24). After complete description of the study to subjects, written informed consent was obtained. The trial consisted of a 12-week acute phase (with a 12-week crossover phase for patients who did not respond), a 16-week continuation phase, and a 76-week maintenance phase (23). All patients entering the trial had a 24-item Hamilton Depression Rating Scale total score of ≥18 after a 1-week, single-blind placebo washout.
Patients excluded from the study were those with DSM-III-R-defined diagnoses of organic mental syndrome; current or lifetime bipolar disorder or cyclothymia; schizophrenia or other psychotic disorder; obsessive-compulsive disorder; antisocial, schizotypal, or severe borderline personality disorder; a principal diagnosis of panic disorder, generalized anxiety disorder, or posttraumatic stress disorder within the past 6 months; anorexia or bulimia nervosa within the past year; or drug or alcohol abuse or dependence within the past 6 months. The protocol criteria excluded individuals who required concomitant therapy with any psychotropic drug (except chloral hydrate or temazepam, used sparingly for sleep disorders) and patients who had failed a previous adequate trial of sertraline or imipramine. Because the intent of the trial was to examine the efficacy of antidepressant medications, psychotherapy was prohibited during the study unless it had been initiated at least 3 months before randomization.
After a complete medical/psychiatric history and physical examination, subjects entered a 1-week, single-blind washout phase and then were randomly assigned to treatment with either sertraline or imipramine in a 2:1 ratio. Assessments of various demographic and socioeconomic characteristics, including educational attainment, were made at baseline. A number of medical and psychosocial measures were collected at various points during the trial (23). Age at onset of major depressive disorder was determined by the Structured Clinical Interview for DSM-III-R (25), which was conducted by a certified rater.
Patients’ response to treatment at various trial milestone points was measured by using the 24-item Hamilton depression scale (administered by investigating physicians or certified trained raters) and the Clinical Global Impression (CGI) improvement and severity measures (always administered by a physician). A satisfactory therapeutic response was defined as an improvement of at least 50% from baseline Hamilton depression scale score, a CGI improvement rating of 1 or 2 (very much or much improved), a total Hamilton depression scale score of ≤15, and a final CGI severity rating of ≤3 (no more than mildly ill). Patients not meeting this definition of therapeutic response were classified as nonresponders.
Various instruments and subscales were employed to measure psychosocial functioning and to compare scores of clinical trial subjects with those from “normal populations,” which were based on community studies (26). We used data from the Medical Outcomes Study Health Status Questionnaire and the Medical Outcomes Study 36-item Short-Form Health Survey (27, 28).
The 635 patients in the clinical trial were stratified into two age groups: those less than age 30 (N=104) and those age 30 or older (N=531) at baseline. The age 30 cutoff was selected to ensure that all subjects had ample opportunity for post-high-school human capital accumulation. Comparisons of categorical variable means were based on Cochran-Mantel-Haenszel chi-square tests, while comparisons of continuous variable means used analysis of variance (ANOVA) F tests. To test whether the onset groups scored below community norms on the various domains of the Short-Form Health Survey instrument, one-tailed ANOVA F tests were performed. Various binary measures of behavioral and educational attainment were used as dependent variables in logistic regressions. Explanatory variables included patient’s current age, age squared, as well as binary variables for gender, onset of major depressive disorder (early versus late), and the interaction between gender and age at onset. Statistical inference in the logistic regressions was based on Wald chi-square tests, and statistical inference in the linear regressions was based on t tests.
U.S. Census Data
The U.S. Census Bureau’s Current Population Survey provides data on the demographic structure and earnings of the population (29). We used data for calendar year 1995, taken from a publicly available CD-ROM, for 83,007 individuals between ages 19 and 70, with nonnegative potential work experience (defined as age minus years of schooling minus 6). We defined an individual as having been in the labor force if 1995 total annual earnings from employment or self-employment were greater than $260 (average $5 per week).
The 0/1 binary variable for labor force participation is specified as the dependent variable in logistic regressions, estimated separately by gender. Conditional on the individual being in the labor force, annual employment earnings are related to the socioeconomic variables; the natural logarithm of annual earnings is the dependent variable in least squares regressions (30). Once estimated, these labor force participation and earnings equations provide the basis for a quantitative evaluation of changes in expected annual earnings (the product of the predicted probability of labor force participation=1 times predicted earnings conditional on labor force participation=1) associated with reductions in educational attainment (human capital accumulation), controlling for other socioeconomic characteristics. The software used for both logistic and ordinary least squares estimation was Stata, version 5.0 (Stata Corp., College Station, Tex.).
The 1995 U.S. Census Bureau’s Current Population Survey data on educational attainment histories of recent cohorts of individuals (between ages 25 and 40 in 1995) were then used to construct educational attainment transition probability matrices, by gender, for the entire U.S. population, which indicated the proportion of individuals who completed successively higher levels of education.
Integration of Clinical Trial and U.S. Census Data
To assess the differential probabilities of educational attainment attributable to age of initial onset of major depressive disorder, the clinical trial data was integrated with U.S. Census Bureau’s Current Population Survey population data. Results from the logistic regressions that related educational attainment of trial subjects to initial age of major depressive disorder onset were used to compute odds ratios for attainment of successively higher levels of education for the U.S. population, separately by age at onset and gender (31). When statistically different from even, these differential odds ratios were applied to the educational attainment transition probabilities for the U.S. male and female populations, based on recent cohorts (ages 25–40 in 1995) in the U.S. Census Bureau’s Current Population Survey data set. Through early-onset major depressive disorder prevalence estimates from the National Comorbidity Survey (15% lifetime prevalence for women by age 21, 8% for men) (2), synthetic education transition probability matrices were constructed for populations who at age 21 had experienced early-onset major depressive disorder, and for those who will have experienced depression after age 21 or will never experience major depressive disorder.
The expected annual future lifetime earnings of the early-onset population at age 21 in 1995 was then computed as a weighted average of expected income by educational attainment, where weights reflected the proportions of those with early-onset major depressive disorder who achieved successively higher levels of post-high-school education. A similar calculation was made for the population at age 21 in 1995 who would be expected to develop major depressive disorder after age 21 or never.
Results
Clinical Trial: Pretreatment Patient Characteristics
Of the 635 trial subjects, 531 were age 30 and over at baseline. Among this subgroup, the 226 patients (42.6%) with early-onset major depressive disorder differed in a number of important ways from the 305 patients (57.4%) with late-onset major depressive disorder. As shown in Table 1, subjects with early onset of major depressive disorder were more likely to be female, to have never married, and to have had a history of alcohol or drug abuse. The early-onset patients were also significantly younger than those patients with late-onset major depressive disorder (mean=41.3 years [SD=7.6] versus 45.7 years [SD=8.4], respectively) (F=6.26, df=1, 529, p<0.001). There was no significant difference between early- and late-onset subjects in employment status, educational attainment, or current type of depression, and the two groups were similar in terms of baseline severity of depression as measured by their Hamilton depression scale scores (mean=24.8 [SD=5.3] and 24.8 [SD=5.6], respectively) (F=0.07, df=1, 529, p=0.95). Almost half (46.0%) of the patients with early-onset major depressive disorder also had a history of early-onset dysthymia, whereas early-onset dysthymia occurred in only 28.5% of the patients with late-onset major depressive disorder.
Levels of educational attainment, whether the patient ever married, and histories of alcohol or drug abuse depended in part on age. To account for possible age confounds, and to permit identification of gender-specific impacts, multivariate logistic regressions were performed. Results of these logistic regressions, expressed in the form of odds ratios, are given in Table 2.
The impact of early-onset major depressive disorder on whether the patient had never married varied by gender. The likelihood of women with early-onset depression never having married was not significantly different from that of women whose onset was later. However, men with early-onset depression were more than twice as likely to have never married than were men whose depressive onset occurred later. While men and women with late-onset major depressive disorder did not differ from each other, men with early-onset depression were more than twice as likely to have never married than were women with early-onset depression. For men, the impact of early-onset major depressive disorder was most apparent on this simple index of intimate relationships.
Impacts of early-onset major depressive disorder on substance abuse also varied by gender. Women with early-onset major depressive disorder were much more likely than those with late-onset depression to have a history of alcohol or drug abuse. Age at onset did not significantly affect the risk of having a history of alcohol or drug abuse for men. The propensity for men to have a history of alcohol or drug abuse was generally larger than that for women. However, although men with late-onset major depressive disorder had an almost fourfold greater risk of alcohol abuse history than women with late-onset depression, the male-female relative risk dropped by about half when both genders had early-onset major depressive disorder.
Although the likelihood of having attended college was unaffected by age at onset, for those who attended college, early-onset major depressive disorder negatively affected the probability of graduating, particularly for women. Women with early-onset major depressive disorder were about half as likely to obtain a college degree as their older-onset counterparts. Further, within the early-onset group, men were almost twice as likely as women to graduate. This large negative impact of early-onset major depressive disorder for women appeared to continue beyond college into graduate studies, as women with early-onset major depressive disorder were half as likely as those with late-onset depression to seek postgraduate training. For men, however, the likelihood of attempting a postgraduate degree was unaffected by age at onset.
In terms of the six domains of psychological functioning measured at baseline by the Short-Form Health Survey, subjects with early- and late-onset major depressive disorder scored significantly lower than the “normal” population in each of the domains (results not shown, one-tailed ANOVA, df=1, 529, all F>20 and p<0.001). Between the early- and late-onset patients, scores were significantly different only for the domains of physical functioning (two-tailed ANOVA, F=6.60, df=1, 529, p=0.01) and work/daily activities—physical (two-tailed ANOVA, F=4.93, df=1, 529, p=0.03), with the late-onset patients having scores on both that indicated greater impairment. Further details are available upon request from the corresponding author (L.M.K.).
Clinical Trial: Treatment Response
Symptomatic treatment responsiveness was independent of age at onset, both in terms of subject attrition during phases of the trial and treatment responsiveness for those who completed a trial phase (Table 3). The likelihood of dropping out during the acute phase, or of dropping out during the continuation or maintenance phase, was not significantly affected by age of major depressive disorder onset or gender; no odds ratio significantly differed from unity. For patients who completed the acute phase, the probability of achieving a satisfactory acute-phase therapeutic response was independent of age at onset. Among the acute-phase responders, age of major depressive disorder onset did not affect the likelihood of maintaining the therapeutic response during the maintenance phase of the trial, although among the subjects with late-onset major depressive disorder, the likelihood was significantly greater for men than for women. The likelihood of patients randomly assigned to receive placebo maintaining a therapeutic response during this trial phase was only one-quarter that of patients randomly assigned to receive sertraline.
Least squares regression estimates, where the dependent variable is the change in Hamilton depression scale score since the beginning of that trial phase (negative implies improvement), and with beginning-phase Hamilton depression scale score as an additional regressor, indicate that the amount of change in Hamilton depression scale score was unaffected by gender or age of major depressive disorder onset. However, during the maintenance phase, being randomly assigned to receive placebo in place of sertraline resulted in a mean 4-point worsening in score on the Hamilton depression scale.
The Short-Form Health Survey results (not shown) suggest that therapeutic responders returned to levels of psychosocial functioning generally comparable to community norms, regardless of major depressive disorder age at onset. In four of the six domains (general health, pain, work/daily activities—physical, and interpersonal functioning), therapeutic responders after the 12-week acute phase were insignificantly different from normal community populations (one-tailed ANOVA, df=1, 529, all F≤1.17 and p≥0.14). In the physical functioning domain, late-onset subjects had slightly but significantly lower scores than the community subjects (one-tailed ANOVA, df=1, 529, F=6.40, p=0.006). In the work/daily activities—emotional domain, both early and late-onset subjects had slightly but significantly lower scores than the community subjects (one-tailed ANOVA, df=1, 529, F=3.25 and F=3.23, p=0.04 for both). In each of the six domains, however, the mean scores of the early- and late-onset patients were not significantly different from each other (two-tailed ANOVA, df=1, 529, all F≤2.96 and p≥0.09). Further details are available upon request from the corresponding author.
Education and Earnings Impacts of Lost Human Capital
The impact of early-onset depression on future earnings arise in our framework because of associated reductions in educational attainment. Trial data indicated that for men, early-onset major depressive disorder did not affect subsequent educational attainment. For women, however, the likelihood of completing a college degree for those attending college was only 57% as high for those with early- versus late-onset major depressive disorder, and for college degree recipients, the odds for pursuing postgraduate training were only 50% as high.
As seen in the final two columns of Table 4, in relation to the female U.S. population in 1995, early-onset major depressive disorder resulted in considerable reductions in highest educational attainment, i.e., in lost human capital. More women with early- than late-onset major depressive disorder attended college but did not complete a college degree program, which resulted in a smaller proportion of early-onset women having a college degree as their highest level of educational attainment.
To assess the earnings impact of reductions in human capital accumulation associated with early-onset major depressive disorder for women, we related 1995 earnings of U.S. women ages 19–70 to levels of educational attainment. Although not shown here, consistent with other labor market studies (30), we found that annual earnings are greater and peak at older ages with successive increases in educational attainment.
When these age at onset, educational attainment, and income data are combined, they reveal significant declines in expected future annual earnings for women experiencing early-onset versus late-onset/never-occurring major depressive disorder. As shown in Figure 1, expected annual earnings at age 35 for two women 21 years of age in 1995 would be $22,461 for the woman with late-onset/never-occurring major depressive disorder but only $19,795 ($2,666, or 11.9% less) for the woman with early-onset major depressive disorder. At age 45, the expected annual earnings gap widens to $26,071 versus $22,341 ($3,730, or 14.3% less), respectively, and at age 55 expected annual earnings are $19,415 versus $15,937 ($3,478, or 17.9% less). We emphasize that these are annual decrements. Were they to be summed over a lifetime in the workforce, these decrements would be more substantial. Thus, early-onset major depressive disorder has considerable consequences for the expected earnings of women.
Discussion
The clinical trial data provide strong empirical support for the hypothesis that early-onset major depressive disorder adversely affects the final educational attainment of young women. Early-onset major depressive disorder does not exhibit a significant effect on the educational attainment of young men. The negative educational attainment effect for women constitutes one form of lost human capital from early-onset major depressive disorder: the expected future earnings of these women with early-onset major depressive disorder are decreased by about 12%–18% relative to women whose onset occurred after age 21 or not at all. While employment rates for patients with early- and late-onset major depressive disorder were similar, the reduced educational attainment of women with early-onset major depressive disorder results in lower expected income.
A second important finding is that both the symptomatic relief and the psychosocial improvement that follow acute-phase and longer-term antidepressant treatment were independent of age of depression onset. As reported elsewhere (24), 60% of the chronically depressed patients who completed the acute phase of this trial were classified as therapeutic responders. The odds of a patient completing the various phases of this trial were independent of age of major depressive disorder onset. Moreover, the psychosocial functioning of therapeutic responders, as measured by various domains of the Short-Form Health Survey, was comparable to community norms regardless of age of major depressive disorder onset.
Together, these findings lead us to conclude that early-onset major depressive disorder causes substantial human capital loss. Early detection and appropriate antidepressant treatment of major depressive disorder among the young could have substantial economic benefits, particularly for women (32).
We have confined our analysis to the economic implications resulting from reduced educational attainment associated with early-onset major depressive disorder. Our analysis does not take into account whether the amount and quality of learning achieved at each education level are affected by early-onset major depressive disorder, as well as any earnings implications of these possible impacts. This study did not assess related effects of early-onset major depressive disorder on human capital formation involving marital status or drug and alcohol abuse, each of which was significantly affected by early-onset major depressive disorder. Moreover, our analysis of the burden of early-onset major depressive disorder did not encompass important noneconomic factors, such as the patients’ satisfaction and quality of life and that of their families and friends.
Because college graduation is more likely to occur by age 22 than age 21, we defined early-onset major depressive disorder as occurring before age 22. Although not reported here, our principal findings are essentially unaffected when early onset is defined as occurring up to age 18 or to age 21 (the DSM-IV definition), rather than to age 22. These findings are robust to other modifications, such as 1) when the older subgroup is categorized as those over age 35, or over age 40, rather than using the age-30 demarcation; 2) when the lifetime prevalence of major depressive disorder for 21-year-old women is 10% or 20%, rather than 15%; or 3) when labor force participation is defined as occurring when annual earnings are several multiples of $260. Moreover, the educational attainment results for women with early- versus late-onset major depressive disorder are unaffected when drug and/or alcohol abuse histories are added as explanatory variables to the logistic regressions.
Our results amplify earlier reported gender differences in dysthymia and chronic major and double depression and buttress the findings of others relating to early-onset chronic depression and comorbidity with selected personality disorders (32–36). There is some evidence that early-onset major depressive disorder is associated with a greater degree of comorbidity than early-onset dysthymia and may represent a more serious form of the disorder (33, 34). The clinical trial data indicated that unlike early-onset major depressive disorder, early-onset dysthymia did not have statistically significant impacts on patients’ marital, substance abuse, or education attainment histories, either when considered by itself or in combination with early-onset major depressive disorder. Whether early-onset dysthymia and major depressive disorder have different impacts on human capital accumulation merits further research.
Several additional caveats should be noted. First, the trial included only subjects with chronic depression. We could not assess whether a single episode of early-onset major depressive disorder with no subsequent relapse or recurrence would have a significant impact on human capital formation. The risks of recurrence and relapse from initial and subsequent episodes of major depressive disorder have been shown, however, to be considerable (37–40). Second, our clinical trial data may understate the impact of chronic depression. Specifically, prospective patients with profound comorbid illnesses or treatment resistance to multiple therapies were not included in the trials. Third, we cannot ascertain whether patients with early-onset major depressive disorder would have responded equally if they had been appropriately treated years earlier at the initial onset of major depressive disorder. However, selective serotonin reuptake inhibitor response rates of young major depressive disorder patients have been shown to be equivalent to those of older subjects (41).
Our results extend available knowledge concerning the impact of undifferentiated recent psychiatric disorders on labor market outcomes (42). Further research into these relationships can provide important inputs into policy discussions on the cost effectiveness of medical care expenditures.
 |
 |
 |
 |
Received Feb. 9, 1999; revisions received July 7, Sept. 9, and Nov. 29, 1999; accepted Dec. 27, 1999. From the Massachusetts Institute of Technology, Cambridge; Stanford University, Stanford, Calif.; the University of Arizona, Tucson; Virginia Commonwealth University, Richmond; Brown University, Providence, R.I.; University of Pittsburgh, Pittsburgh; the University of Texas Southwestern Medical Center at Dallas; and the VA Medical Center, Dallas. Address reprint requests to Dr. Koran, OCD Clinic Room 2363, 401 Quarry Rd., Stanford, CA 94305. This study was supported by Pfizer Inc. The authors thank Howard Birnbaum, Paul E. Greenberg, Amy Grudzinski, James M. Russell, and Jason Verner for their assistance with this study.
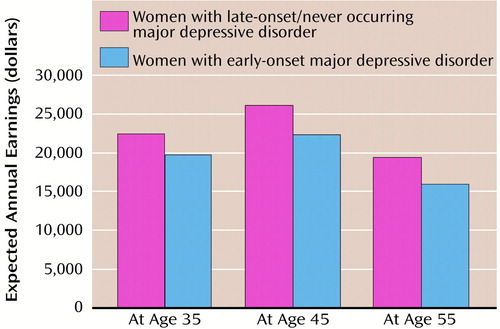
Figure 1. >Expected Mean Annual Earnings for Women With Early-Onset Major Depressive Disorder Versus Those of Women With Late-Onset/Never-Occurring Major Depressive Disordera
aEarly onset=before age 22; late onset=at age 22 or later. Bars represent the average earnings a 21-year-old woman in 1995 could expect to receive in the future depending on the presence and age at onset of major depressive disorder.
1. Becker GS: Human Capital: A Theoretical and Empirical Analysis, With Special Reference to Education. New York, National Bureau of Economic Research, 1964Google Scholar
2. Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB: Sex and depression in the National Comorbidity Survey, I: lifetime prevalence, chronicity and recurrence. J Affect Disord 1993; 29:85–96Crossref, Medline, Google Scholar
3. Broadbent WE, Blazer DG, George LK, Tse CK: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 1990; 264:2524–2528Google Scholar
4. Conti DJ, Burton WN: The economic impact of depression in a workplace. J Occup Med 1994; 36:983–988Medline, Google Scholar
5. Greenberg PE, Kessler RC, Nels TL, Finkelstein SN, Berndt ER: Depression in the workplace: an economic perspective, in Selective Serotonin Reuptake Inhibitors: Advances in Basic Research and Clinical Practice, 2nd ed. Edited by Feighner JP, Boyers WF. Chichester, UK, John Wiley & Sons, 1996, pp 321–358Google Scholar
6. Wells KB, Stewart AL, Hays RD, Burnam MA, Rogers WH, Daniels M, Berry S, Greenfield S, Ware JE Jr: The functioning and well-being of depressed patients. JAMA 1989; 262:914–919Crossref, Medline, Google Scholar
7. Klerman GL: Depressive disorders: further evidence for increased medical morbidity and impairment of social functioning. Arch Gen Psychiatry 1989; 46:856–858Crossref, Medline, Google Scholar
8. Hays RD, Wells KB, Sherbourne CD, Rogers WH, Spritzer K: Functioning and well-being outcomes of patients with depression compared with chronic general medical illness. Arch Gen Psychiatry 1995; 52:11–19Crossref, Medline, Google Scholar
9. Wells KB, Sturm R, Sherbourne CD, Meredith LS: Caring for Depression. Cambridge, Mass, Harvard University Press, 1996Google Scholar
10. Wells KB, Hays RD, Burnham MA, Rogers WH, Greenfield S, Ware JE Jr: Detection of depressive disorder for patients receiving prepaid or fee for service practices; results from the Medical Outcomes Study. JAMA 1989; 262:925–930Crossref, Medline, Google Scholar
11. Katon W, Von Korff M, Lin EHB, Bush T, Ormel J: Adequacy and duration of antidepressant treatment in primary care. Med Care 1992; 30:67–76Crossref, Medline, Google Scholar
12. Keller MB, Klerman GL, Lavori PW, Fawcett JA, Coryell WA, Endicott J: Treatment received by depressed patients. JAMA 1982; 248:1848–1855Google Scholar
13. Keller MB, Lavori PW, Klerman GL, Andreasen NC, Endicott J, Coryell W, Fawcett J, Rice JP, Hirschfeld RM: Low levels and lack of predictors of somatotherapy and psychotherapy received by depressed patients. Arch Gen Psychiatry 1986; 43:458–466Crossref, Medline, Google Scholar
14. Keller MB: Undertreatment of major depression. Psychopharmacol Bull 1988; 24:75–80Medline, Google Scholar
15. Kocsis JH, Frances AJ, Voss C, Mann JJ, Mason BJ, Sweeney J: Imipramine treatment for chronic depression. Arch Gen Psychiatry 1988; 45:253–257Crossref, Medline, Google Scholar
16. Keller MB, Harrison WM, Fawcett JA, Gelenberg AJ, Hirschfeld RMA, Klein D, Kocsis JH, McCullough JP, Rush AJ, Schatzberg AF, Thase ME: Treatment of chronic depression with sertraline or imipramine: preliminary blinded response rates and high rates of undertreatment in the community. Psychopharmacol Bull 1995; 31:205–212Medline, Google Scholar
17. Perez-Stable EJ, Miranda J, Munoz RF, Ying YW: Depression in medical outpatients: underrecognition and misdiagnosis. Arch Intern Med 1990; 150:1083–1088Google Scholar
18. Regier DA, Hirschfeld RMA, Goodwin FK, Burke JD Jr, Lazar JB, Judd LL: The NIMH Depression Awareness, Recognition and Treatment Program: structure, aims, and scientific basis. Am J Psychiatry 1988; 145:1351–1357Google Scholar
19. Baldessarini RJ: Current status of antidepressants: clinical pharmacology and therapy. J Clin Psychiatry 1985; 50:117–126Google Scholar
20. American Psychiatric Association: Practice Guideline for Major Depressive Disorder in Adults. Am J Psychiatry 1993; 150(April suppl)Google Scholar
21. Kupfer DJ, Frank E, Perel JM, Cornes C, Mallinger AC, Thase ME, McEachran AB, Grochocinski VJ: Five year outcomes for maintenance therapies in recurrent depression. Arch Gen Psychiatry 1992; 49:769–773Crossref, Medline, Google Scholar
22. Keller MB, Kocsis JH, Thase ME, Gelenberg AJ, Rush AJ, Koran LM, Schatzberg AF, Russell JM, Hirschfeld RMA, Klein DN, McCullough JP, Fawcett JA, Kornstein SM, LaVange L, Harrison WM: Maintenance phase efficacy of sertraline for chronic depression, a randomized controlled trial. JAMA 1998; 280:1665–1672Google Scholar
23. Rush AJ, Koran LM, Keller MB, Markowitz JC, Harrison WM, Miceli RJ, Fawcett JA, Gelenberg AJ, Hirschfeld RMA, Klein DN, Kocsis JH, McCullough JP, Schatzberg AF, Thase ME: The treatment of chronic depression, part 1: study design and rationale for evaluating the comparative efficacy of sertraline and imipramine as acute crossover, continuation, and maintenance phase therapies. J Clin Psychiatry 1998; 59:589–597Crossref, Medline, Google Scholar
24. Keller MB, Gelenberg AJ, Hirschfeld RMA, Rush AJ, Thase ME, Kocsis JH, Markowitz JC, Fawcett JA, Koran LM, Klein DN, Russell JM, Kornstein SG, McCullough JP, Davis SM, Harrison WM: The treatment of chronic depression, part 2: a double-blind, randomized trial of sertraline and imipramine. J Clin Psychiatry 1998; 59:598–607Crossref, Medline, Google Scholar
25. Spitzer RL, Williams JBW, Gibbon M, First MB: The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 1992; 49:624–629Crossref, Medline, Google Scholar
26. Miller IW, Keitner GI, Schatzberg AF, Klein DN, Thase ME, Rush AJ, Markowitz JC, Schlager D, Kornstein SG, Davis SM, Harrison WM, Keller MB: The treatment of chronic depression, part 3: psychosocial functioning before and after treatment with sertraline or imipramine. J Clin Psychiatry 1998; 59:608–617Crossref, Medline, Google Scholar
27. Tarlov AR, Ware JE Jr, Greenfield S, Nelson EC, Perrin E, Zubkoff M: Medical Outcomes Study: an application of methods for evaluating the results of medical care. JAMA 1989; 262:907–913Crossref, Medline, Google Scholar
28. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473–483Crossref, Medline, Google Scholar
29. US Bureau of the Census: Current Population Survey: Current Population Reports, Series P-20 and P-60. Washington DC: US Government Printing Office, March 1997Google Scholar
30. Berndt ER: Analyzing determinants of wages and measuring wage discrimination: dummy variables in regression models, in The Practice of Econometrics: Classic and Contemporary. Edited by Berndt ER. Reading, Mass, Addison-Wesley, 1991, pp 150–223Google Scholar
31. Kocsis JH, Frances AJ, Voss C, Mason BJ, Mann JJ, Sweeney J: Imipramine and social-vocational adjustment in chronic depression. Am J Psychiatry 1988; 145:997–999Link, Google Scholar
32. Kornstein SG, Schatzberg AF, Thase ME, Yonkers KA, McCullough JP, Keitner GI, Gelenberg AJ, Ryan CE, Hess AL, Harrison WM, Davis SM, Keller MB: Gender differences in chronic major and double depression. J Affect Disord (in press)Google Scholar
33. Fava M, Alpert JE, Borus JS, Nierenberg AA, Pava JA, Rosenbaum JF: Patterns of personality disorder comorbidity in early-onset versus late-onset major depression. Am J Psychiatry 1996; 153:1308–1312Google Scholar
34. Kash KL, Klein DN: The relationship between age at onset and comorbidity in psychiatric disorders. J Nerv Ment Dis 1996; 184:703–707Crossref, Medline, Google Scholar
35. Rohde P, Lewinsohn PM, Seeley JR: Comorbidity of unipolar depression, II: comorbidity with other mental disorders in adolescents and adults. J Abnorm Psychol 1991; 100:214–222Crossref, Medline, Google Scholar
36. Klein DN, Schatzberg AF, McCullough JP, Keller MB, Dowling F, Goodman D, Howland RH, Markowitz JC, Smith C, Miceli RJ, Harrison WM: The early versus late distinction in dysthymic disorder: comparison on demographic and clinical variables, family history, and treatment response in outpatients with superimposed major depressive episodes. J Affect Disord 1999; 52:187–196Crossref, Medline, Google Scholar
37. Keller MB, Shapiro RW, Lavori PW, Wolfe N: Recovery in major depressive disorder. Arch Gen Psychiatry 1982; 39:905–910Crossref, Medline, Google Scholar
38. Keller MB, Lavori PW, Endicott J, Coryell W, Klerman GL: “Double depression”: two-year follow-up. Am J Psychiatry 1983; 140:689–694Link, Google Scholar
39. Keller MB, Klerman GL, Lavori PW, Coryell WA, Endicott J, Taylor J: Long-term outcome of episodes of major depression. JAMA 1984; 252:788–792Crossref, Medline, Google Scholar
40. Keller MB, Lavori PW, Rice JB, Coryell W, Hirschfeld RMA: The persistent risk of chronicity in recurrent episodes of nonbipolar major depressive disorder: a prospective follow-up. Am J Psychiatry 1986; 143:24–28Link, Google Scholar
41. Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Hughes CW, Carmody T, Rintelman J: A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997; 54:1031–1037Google Scholar
42. Ettner SL, Frank RG, Kessler RC: The impact of psychiatric disorders on labor market outcomes. Ind Labor Relat Rev 1997; 51:64–81Crossref, Google Scholar